UMBC researcher Govind Rao wants to bring the bounty of the information age to a drugstore near you.
By Joab Jackson ’90
“You’re watching history being made.”
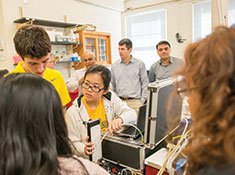
I am in the basement of UMBC’s Center for Advanced Sensor Technology (CAST), speaking with its director, Govind Rao. The “history” that Rao speaks of is a large metallic suitcase, filled with snaking tubes and strange components, being attended to by a swarm of graduate students.
The suitcase is an early prototype of a device that might, one day, be able to produce many medicines the world needs. What’s happening in this basement might radically change a $300 billion health care industry.
Rao is leading 30 people to build the device, as part of a project called BioMOD, short for “biologically-derived medicines on demand.” The U.S. Defense Advanced Research Projects Agency (DARPA) has funded CAST with a $15.7 million grant over four years to make the device happen.
The heart of the unit is a “bioreactor,” which combines a dried extract of cellular machinery with specific DNA to create the medicine that is needed. The unit is also filled with other equipment to warm the resulting combination to the required temperature, as well as purify the mixture into medicine that can be placed in syringes or vials.
“The goal is to replace an acre-sized plant costing a billion dollars and taking three months to ship out medicine,” says Rao, “with a suitcase sized device” that can produce medicines where they are needed – be it a disaster zone, or a battlefield, or even a far-flung community.
USEFUL DISRUPTIONS
It might seem strange that one can make history in the Technology Research Center – a small complex of buildings at the southeast edge of UMBC’s campus with roots as a juvenile detention center. But Rao and his colleagues at CAST have a knack for creating innovation in unlikely places.
“Only the inmates have changed,” jokes Rao, who is also a professor of biochemical, chemical, and environmental engineering at the university. Rao began his career in chemical engineering, a field that remains his first love. After earning his Ph.D. at Drexel University, he arrived at UMBC in 1987 and has been here ever since. In the almost 30 years Rao has been on campus, CAST has grown from a hybrid of researchers from the University of Maryland Biotechnology Institute and the Center for Fluorescence Spectroscopy into a fully-fledged research center within UMBC that attracts affiliated faculty from numerous departments and centers on campus.
The primary focus of CAST has been the creation of novel sensor technologies, with a dizzying array of patents, publications and projects to its credit. But Rao says the center is determined to discover broader ways to help humanity with the work it accomplishes.
“I never thought I’d stay here for as long as I have,” says Rao. “But [UMBC] has everything I need nearby.”
UMBC’s location has been a boon for Rao and his center. The headquarters for many of the agencies, companies, and fellow academic institutions he deals with are nearby, as is BWI Airport. The U.S. Food and Drug Administration and the U.S. Department of Agriculture are also nearby, as are the University of Maryland and The Johns Hopkins University. Experts in many areas relevant to the center are a short drive or flight away.
Creating a space where research and public policy come into confluence has helped CAST thrive. And the desire to make a real-world impact has also led the center to its current focus on medicines.
Rao says the center is always looking for “disruptive innovations leading to paradigm shifting practices.” He thinks the health care industry is ripe for such a shift. Reducing the skyrocketing costs of health care will not only relieve pressures on consumers in the U.S. and elsewhere, but might also make health care innovations that are currently cost-prohibitive for developing countries available to their populations as well.
Rao sees a powerful precedent in the computer industry. In the 1960s, the world’s computer power was concentrated in a handful of expensive mainframes. Today, nearly everyone holds the power of yesterday’s mainframes within their relatively low-cost smartphones, more than a billion of which are now in use.
While it might be harder to bring the same decentralization to an industry as powerful and as heavily regulated as health care, Rao sees the effort to do so as essential in a moment when the average yearly cost of health care in the United States citizen is approaching $10,000 per person – one of the highest costs of any country in the world.
“If you look at the trend lines, health care costs will continue to steeply rise,” says Rao.
Rao was first nudged to make a link between his previous research and rising pharmaceutical costs by Steve Falk, chief engineer for maternal health care technologies at General Electric’s health care division. When he toured the CAST lab a few years ago, Falk noticed a poster about a molecule that changed brightness depending on its temperature. Falk’s mind made a jump to the medical uses for such a molecule, and suggested to Rao a possible link between his technology and the ongoing problem of infant mortality. Despite many advances in prenatal and postnatal care, a baby still dies every 10 seconds around the world.
Falk says Rao ran with the idea, seeking out opportunities to build low-cost technologies to boost infant care. The team at CAST was especially eager to develop opportunities for care for those in poor or rural areas that lack doctors and high-tech facilities.
Creating a more baby-friendly way of checking blood sugar levels was among the first projects the center pursued. Checking an infant’s glucose level is done at present with a heel “stick” where a needle is used to prick the baby’s heel and collect a blood sample. But since a newborn baby has a very small blood volume, each heel stick is costly in terms of pain and risk of anemia, not to mention the risk of infection.
When considering the problem, Rao and his team focused on the fact that a baby’s skin, especially if it is premature, is much thinner than an adult’s skin. In fact, it proved to be thin enough that glucose would readily diffuse across it and allow one to measure the blood sugar level of the infant without a prick.
The CAST researchers then developed a non-invasive sensor to replace the heel stick. A chamber is placed on the skin and allows blood components, such as glucose, oxygen or carbon dioxide to diffuse into it. One could then shine a light on the chamber, and the reflected light would indicate the level of each of these substances.
This non-invasive approach could also be used for other measurements, and be adapted for use in adults. Rao envisions the eventual creation of a handheld device – not dissimilar in appearance from the “tricorder” used by medical officers in Star Trek – that might detect a wide range of medical conditions.
CAST is also working on a separate project, powered by undergraduate students, to develop a low-cost babywarmer, built from cardboard and a heater. The collapsible and disposable box addresses concerns about adequate cleaning in low-cost settings while keeping the baby warm using a minimum of technology. Students are now working to outfit the box with low-powered sensors to collect and record the infant’s vital signs.
LIGHT BULB MOMENTS
Rao calls projects such as the baby warmer “frugal innovation.” But the “suitcase” that the center is developing for BioMOD is CAST’s most ambitious and complex project yet.
Col. Geoffrey Ling, former director of the Biological Technologies Office at DARPA, came up with the idea for BioMOD, which he discussed in an agency meeting attended by Rao.
Ling, a practicing neuro-intensivist caring for severely injured military personnel, completed a total of five tours of duty in Afghanistan and Iraq. During those tours, he had found it difficult to get the medicines he needed in either combat zone. He wanted a device that could produce any medicine – on-demand and within a 24-hour period.
“He pretty much said that he wanted to put the current pharmacy business model of centralized production and distribution out to pasture,” Rao recalls.
It was a radical statement, and Rao started out by pondering the sheer impossibility of such a device. The timeline for making a medicine also did not seem feasible, at least initially. It takes a mammalian cell about 20 hours to divide, assuming those cells could be kept alive for that period of time in the first place. Currently, many biologically-based medicines are produced in cell culture by introducing DNA for a desired product into living cells or bacteria; these then make the product, which then needs to be isolated and purified. The whole process can take days to weeks.
But a short time later, Rao ran across an ad in a trade publication from a biotechnology company called Thermo Fisher Scientific. The company had technology that could strip a nucleus from a cell but preserve all the “machinery” needed to make a protein, simply by adding DNA to the extract. This “machinery” or cell-free extract was available as a freeze-dried powder and most importantly, provided a way around the problem of keeping cells alive in order to make protein.
“That was sort of the light bulb moment for me,” says Rao.
Rao assembled a cross-disciplinary team, including students and faculty from most of UMBC’s engineering departments, in addition to the chemistry and biological science departments, and UMB’s pharmacy department to harness the cell-free technology and combine it with the fluidics, and control and purification systems necessary to build a device capable of producing medicines on demand. A purification expert from Ohio State University was recruited, as well as a group of system integrators from the Latham BioPharm Group to manage the complex project.
The team has built a working prototype that can be loaded with a freeze-dried cellular extract of Chinese hamster ovary (CHO) cells, which are what the pharmaceutical industry often uses to produce medicines. The idea is that the CHO cell extract, which does not contain nuclei, remains inert until the bioreactor infuses it with the necessary DNA, water, and a few chemicals. Once activated, the process should take only a few hours to produce a medicine ready to inject into a human.
“Most modern biological medicines are proteins,” Rao said. “They are either antibodies or they are enzymes that have very specific activities that modulate cellular functions.” Bio-MOD could be used to make erythropoietin, for instance, which boosts production of red blood cells.
The next major challenge for BioMOD will be to get the device to produce medicines with sufficient consistency, purity, and potency to make the Food and Drug Administration comfortable in approving the technology for public use.
“That’s a pretty high bar,” Rao admits. Rigorous clinical trials and corporate backing of some sort will likely be required to clear it.
Yet the potential is enormous. Now that medical science has arrived at the point where each individual’s genome can be sequenced, medicines could be tailor-made for each person. A patient with diabetes, for instance, could have a personalized cocktail of antibodies and proteins such as insulin that address the specific quirks of their condition and their DNA.
Rao says that CAST’s “pharmacy in a box” “is one of those enabling technologies like 3-D printing. I don’t know where it will go.”
Though the ambitions of CAST continue to grow, Rao keeps a lean outfit at the center. “My secret to making all this happen is all about getting the right people, with shared core values,” he said.
The center operates with a relatively flat management structure. Team members are encouraged to question authority, stray outside their comfort zones, and avoid what Rao calls “pride of expertise.”
Rao observes” If you’re not comfortable dealing with someone from a different discipline or with a different approach, it gets in the way of true innovation.”
Though the center has had many successes, CAST also has a high tolerance for failure. “If you do not fail, you are not trying” is another core principle in Rao’s model. “I am nothing without my team. We rise and fall together,” says Rao.
GE’s Falk says Rao “has the vision, but he also can move the team in the same direction. Everyone feels included, and all of a sudden, you have a team that is bigger than you once had, and everyone is rowing in the same direction.”
Tags: Winter 2016